Pearland & Lake Jackson Claudication Clinic
Understanding Claudication: Key Insights into Causes, Symptoms, and Management
Claudication is a symptom often overshadowed by its medical complexity, yet its impact on daily life can be profound. This condition is characterized by pain and cramping in the leg muscles triggered by inadequate blood flow during physical activities such as walking or exercising. Commonly linked to peripheral vascular disease, particularly peripheral artery disease (PAD), claudication not only restricts mobility but also signals significant vascular health issues.
In this article, we delve into the dual nature of claudication—vascular and neurogenic—exploring its roots in both circulatory and spinal health issues. We will unravel the causes behind this painful condition, identify its typical symptoms, and discuss diagnostic approaches and management strategies to maintain quality of life and improve vascular health. To receive expert care and further insight into managing claudication, visiting the Coastal Vascular Center can be an invaluable step for patients, caregivers, or anyone seeking to expand their knowledge and manage the impact of this condition.
What is Claudication?
Claudication is a symptom, not a disease. It’s a telltale sign of peripheral vascular disease, which affects blood vessels outside the heart and brain. This condition primarily impacts the arteries in the legs.
The hallmark of claudication is leg pain or cramping during physical activity. Activities like walking can become challenging. This pain typically eases with rest as the muscles’ demand for blood decreases.
The two primary forms of claudication include:
- Vascular Claudication: Often indicative of significant blood circulation issues, particularly related to peripheral artery disease.
- Neurogenic Claudication: Stemming from complications within the spine and nervous system.
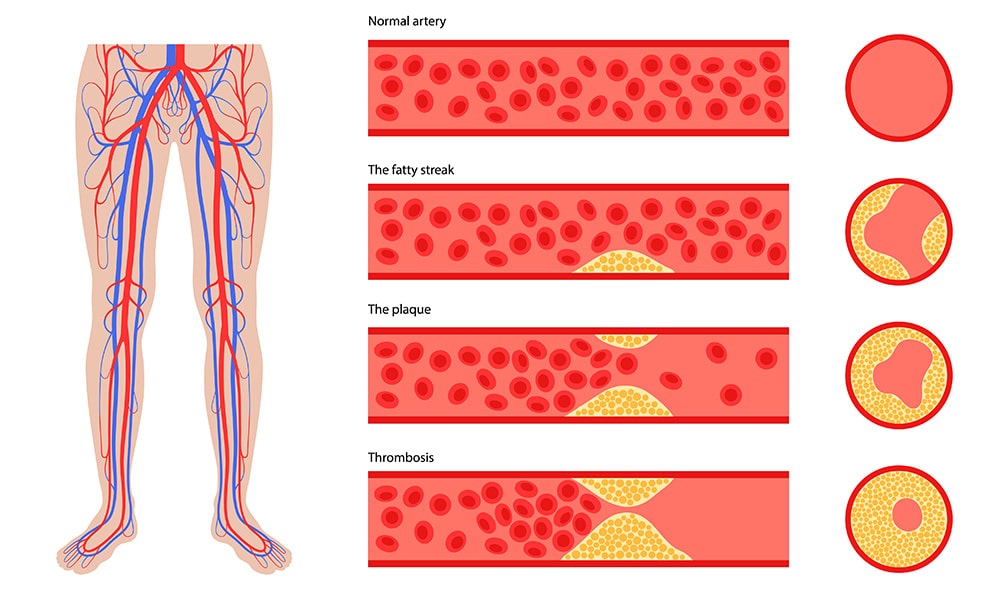
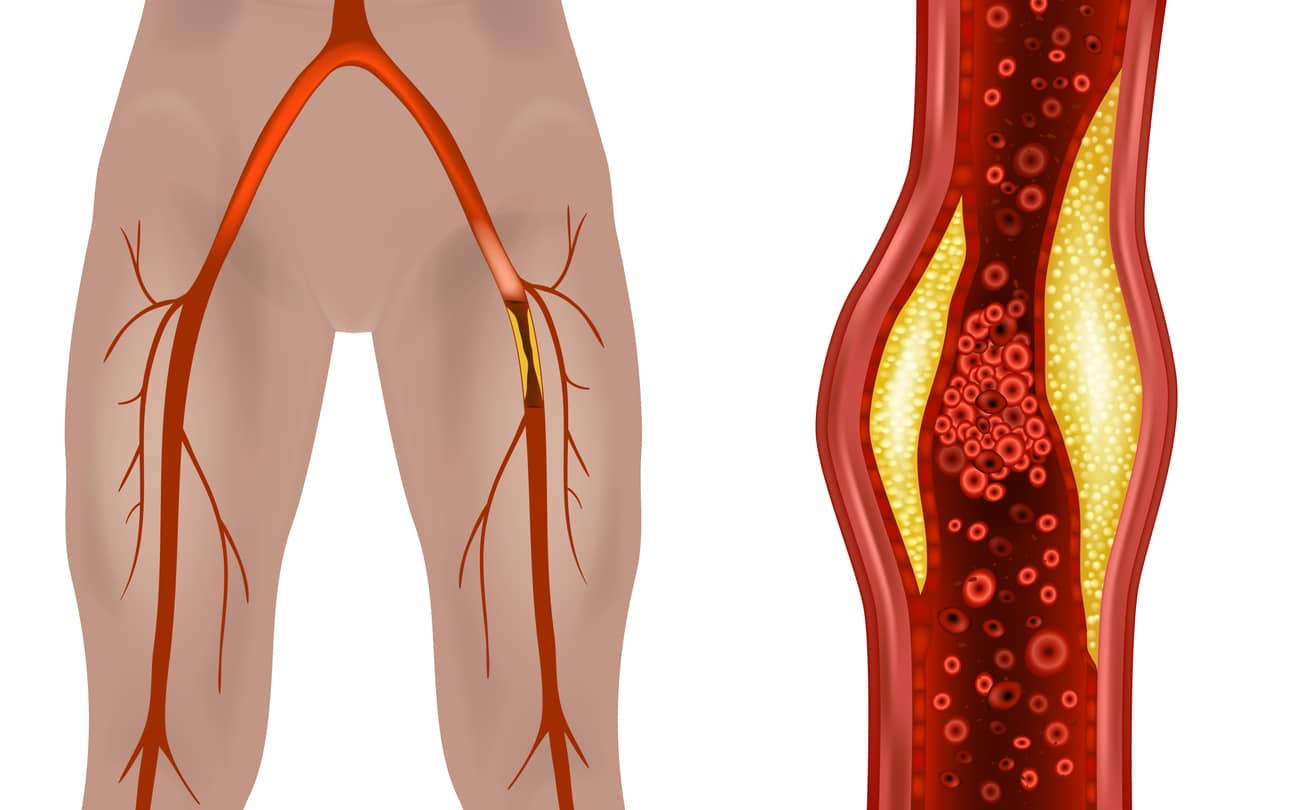
The main issue in claudication is reduced blood flow. When leg muscles don’t receive adequate oxygen-rich blood, they cannot function efficiently, leading to discomfort. This limited blood flow is often due to atherosclerosis, where plaque builds up in arteries, narrowing or blocking them.
Understanding the experience of claudication can be very useful. Here are key points to keep in mind:
- Claudication results from impaired blood flow to leg muscles.
- Pain usually occurs during activities such as walking or climbing stairs.
- Symptoms may subside with rest, only to return upon resumption of activity.
Recognizing these patterns is essential for addressing the symptoms and preventing further complications. Early diagnosis and intervention can improve outcomes and help maintain an active lifestyle.
Schedule Your Vascular Health Check-Up
Don’t let claudication dictate your mobility and quality of life. Proactivity is key. Book an appointment with Dr. Ayar at the Coastal Vascular Center or your local healthcare provider today. Getting an expert evaluation at the earliest sign of discomfort ensures timely treatment and management of your symptoms. Remember, early detection can lead to better outcomes.
Recognizing the Symptoms of Claudication
Claudication might seem elusive at first. Its key symptom is discomfort that surfaces in the legs during physical exertion. This feeling is commonly articulated as a persistent ache, a debilitating cramp, or an unusual sensation of heaviness burdening the leg muscles. This discomfort typically emerges amid walking or exercise and dissipates with adequate rest.
While the discomfort often originates in the calf muscles, it’s not uncommon for it to radiate into the thighs or even the gluteal region. One may notice that the threshold for pain decreases over time; as claudication progresses, ever-decreasing exertion levels could provoke the pain.
For a more thorough understanding of claudication, here are some indicative symptoms to be aware of:
- Muscle discomfort or cramping: Triggered by activity, this pain directly results from diminished blood flow.
- Intermittent numbness or weakness: These leg sensations during activities may signify nerve involvement or severe arterial blockage.
- Temperature disparities: A distinct coldness in the lower leg or foot compared to the other limb might suggest compromised circulation.
- Delayed healing of extremity wounds: Sores or wounds on the toes, feet, or legs that do not recover at a typical pace could indicate insufficient blood supply.
- Erectile dysfunction: In some men, claudication may coincide with erectile dysfunction, revealing a broader scope of arterial disease.
These symptoms vary widely in their intensity. While they may be mild and merely inconvenient for some, they can escalate to crippling pain that may severely limit day-to-day mobility for others. Attentively monitoring these symptoms is essential; without proper medical intervention, they could gradually intensify.
Early detection of claudication symptoms is pivotal. Timely medical consultation, possibly at specialist facilities like the Coastal Vascular Center, along with instituting lifestyle changes, can effectively manage this condition. Such proactive steps aid in averting more severe vascular complications, enhancing the overall quality of life for those affected.
Risk Factors for Developing Claudication
Claudication is often linked to specific risk factors that increase its likelihood. Understanding these factors can aid in prevention and management. Identifying and addressing them is crucial to reducing one’s risk of developing this condition.
Certain lifestyles and health conditions can elevate the risk of claudication. Individuals who smoke, have diabetes, or suffer from high cholesterol levels are more susceptible. Hypertension, or high blood pressure, also plays a significant role in its development.
Here are some significant risk factors for claudication:
- Smoking, which damages blood vessels and impairs circulation
- Diabetes a condition that affects blood flow and nerve function
- High cholesterol, leading to plaque buildup in arteries
- Hypertension, increasing strain on arterial walls
- Advanced age, typically over 50, when blood vessels may narrow
- Sedentary lifestyle, which reduces circulatory efficiency
Addressing these risk factors is essential for prevention. Lifestyle changes and medical management can significantly reduce the risk of developing claudication. Making healthy choices helps maintain vascular health and minimizes potential complications.
The Underlying Causes of Claudication
Understanding claudication requires a closer look at what restricts blood flow in the arteries. The primary culprit is often atherosclerosis, a condition in which plaque, consisting of fat, cholesterol, and other substances, builds up inside the artery walls. This plaque narrows the arteries over time.
As arteries narrow, they obstruct the movement of oxygen-rich blood to the leg muscles. During physical activity, these muscles demand more oxygen than they receive. This imbalance between supply and demand triggers the painful symptoms of claudication.
Other factors may contribute to the development of claudication:
- Genetics: A family history of vascular disease could increase risk.
- Age: Older individuals are more likely to have arterial narrowing.
- Lifestyle: Sedentary behavior and poor dietary habits can exacerbate arterial issues.
Other health conditions can also play a role. High cholesterol, high blood pressure, and diabetes can all elevate the risk of arterial damage. Smoking is another major contributor, as it accelerates the process of atherosclerosis, further restricting blood flow.
Understanding these underlying causes is vital. It helps identify individuals at risk and allows for preventive measures that can slow the progression of claudication. Based on these risk factors, making informed lifestyle changes can greatly enhance vascular health.
What Triggers Vascular Claudication?
Every cell in the body requires oxygen to operate efficiently. Muscle cells demand more oxygen to function during physical activity, even something as mild as a leisurely walk. Increased activity can lead to discomfort for individuals with circulation issues due to insufficient oxygen supply in their bloodstream. This problem resolves upon resting as the demand for oxygen decreases. This discomfort is primarily experienced in the legs but can also occur in the arms.
Vascular claudication is a hallmark indicator of peripheral artery disease (PAD), characterized by the narrowing of blood vessels in the legs, and atherosclerosis, the hardening of the arteries. Both of these conditions elevate the risk of heart attacks and strokes.
Moreover, claudication can discourage physical activity because of the pain it causes during movement, potentially exacerbating the condition.
What Causes Neurogenic Claudication?
Neurogenic claudication usually results from spinal stenosis, also known as pseudo claudication, which narrows spaces in the lower spine. This condition can exert direct pressure on the spinal cord or impinge on the vascular structures surrounding the spine, limiting the oxygen supply. Symptoms may include pain radiating from the lower back down through the legs, along with leg and foot weakness, tingling, or numbness. Additionally, it may affect bowel or bladder control.
A distinctive feature of neurogenic claudication, compared to vascular claudication, is the symptomatic relief experienced when leaning forward, often referred to as the “shopping cart sign.” This posture, likened to pushing a shopping cart, offers pain relief not typically found in cases of vascular claudication.
Diagnosing Claudication: What to Expect
Diagnosing claudication involves several steps to determine its cause and severity. Proper diagnosis is crucial for effective treatment. Healthcare providers use physical assessments and diagnostic tests to identify claudication.
During the diagnostic process, your doctor will perform a thorough evaluation. They will assess your symptoms and check the strength of your leg pulses, which will help them understand the blood flow patterns in the affected areas.
Here are standard methods used to diagnose claudication:
- Physical examinationto assess symptoms and blood flow.
- Medical history reviewto identify underlying conditions and lifestyle factors.
- Ankle-Brachial Index (ABI) testcompares your ankle and arm blood pressure.
- Ultrasoundimaging to visualize blood flow and detect blockages.
- Angiographyto provide detailed images of blood vessels.
Accurate diagnosis allows for tailored treatment options. Early detection and treatment can prevent the condition from worsening.
Physical Examination and Medical History
Your doctor will begin with a physical exam and review of your medical history. They will note symptoms, lifestyle habits, and any underlying medical conditions. This information provides a comprehensive understanding of your vascular health.
Ankle-Brachial Index (ABI) Test
The ABI test is a simple, noninvasive method for diagnosing claudication. It measures blood pressure at the ankle and arm. A lower ABI ratio indicates reduced blood flow to the legs, suggesting possible arterial narrowing.
Imaging Tests: Ultrasound and Angiography
Ultrasound imaging helps visualize blood flow through the arteries and detect blockages. It uses sound waves to provide a real-time picture of vascular health. This non-invasive test helps pinpoint the location of any obstruction.
In more complex cases, angiography may be needed for detailed imaging. This involves injecting contrast dye into blood vessels to view them on X-ray images. It provides a clear and accurate assessment of the severity and location of blockages. These tests are key in planning the most effective treatment strategy.
Treatment Options for Claudication
Treating claudication involves a combination of lifestyle changes, medication, and sometimes surgery. The goal is to improve blood flow and reduce symptoms. Treatment is tailored to the severity of your condition and overall health.
Patients often start by making lifestyle modifications, which can significantly improve symptoms and overall vascular health. Regular exercise, such as supervised walking programs, is commonly recommended.
Medication can also be vital in managing claudication. It enhances circulation and decreases pain during activity. In more severe cases, surgical options may be considered to restore blood flow.
Here are the common treatment methods for claudication:
- Lifestyle changes, including diet and smoking cessation.
- Regular exerciseto promote circulation.
- Medicationsto improve blood flow.
- Surgical interventionsfor advanced cases.
- Dietary modificationsto reduce cholesterol.
Effective management of claudication often requires a combination of these approaches to optimize outcomes.
Lifestyle Changes and Exercise
Adopting a healthier lifestyle is crucial for managing claudication. Stopping smoking is essential to reduce further vascular damage. Incorporating a balanced diet helps maintain healthy cholesterol and weight levels.
Exercise is a cornerstone of claudication treatment. Programs focusing on walking can help increase pain-free walking distances. Regular aerobic activities enhance circulation and strengthen leg muscles, effectively reducing symptoms.
Medications to Improve Blood Flow
Certain medications can alleviate claudication symptoms. These medications are commonly prescribed to improve walking distance by enhancing blood flow.
These medications target symptom relief but do not cure the underlying condition. They are often used in conjunction with lifestyle modifications. Discuss any new medication regimen with your healthcare provider to ensure safety and effectiveness.
Surgical Interventions
When other treatments are ineffective, surgical options may be necessary. Angioplasty is a minimally invasive procedure that widens narrowed arteries. It involves inflating a tiny balloon inside the vessel to restore blood flow.
In more severe cases, vascular surgery might be required. This procedure involves bypassing blocked arteries to improve circulation. Surgery can significantly enhance quality of life, but it requires careful consideration and evaluation by your doctor.
Managing Claudication: Practical Tips and Advice
Successfully managing claudication requires adopting practical everyday strategies. Patients benefit from adjusting in their daily routines. These changes help improve symptoms and promote vascular health.
Committing to lifestyle changes can significantly impact your symptoms and quality of life. Staying active, eating well, and caring for your feet are crucial for managing this condition. Don’t hesitate to consult your healthcare provider for tailored advice.
Consider implementing these practical steps to aid your claudication management:
- Maintain regular physical activity.
- Follow a balanced and heart-healthy diet.
- Prioritize foot care and monitor any skin changes.
- Manage stress through relaxation techniques.
- Keep regular medical appointments and track progress.
These tips can enhance your ability to manage claudication effectively and improve your overall well-being.
Incorporating Physical Activity Safely
Physical activity is essential but must be approached with caution. Start with low-impact exercises like walking or cycling. Gradually increase intensity and duration as your tolerance improves.
Ensure you wear comfortable shoes to support your feet. If you experience pain, stop and rest. It’s vital to avoid pushing beyond your limits. Please consult your healthcare provider before starting any new exercise program to ensure it’s safe for you.
Diet and Nutrition for Vascular Health
A healthy diet is pivotal in managing claudication. Focus on foods rich in fiber, such as whole grains, fruits, and vegetables. These help maintain healthy cholesterol levels and weight.
Limit your intake of saturated fats, trans fats, and salt. Opt for lean proteins and healthy fats, such as omega-3s from fish. Staying hydrated and moderating alcohol can also benefit your cardiovascular health. Remember, dietary changes should be sustainable for lasting benefits.
Foot Care and Preventing Complications
Proper foot care is vital for those with claudication. If injuries are left unchecked, poor circulation can lead to complications. Inspect your feet daily for signs of sores or changes in color.
Wear well-fitted footwear to protect your feet from injury. Keep your skin moisturized to prevent cracking. Be cautious when trimming nails to avoid cuts. If you notice persistent issues, consult a healthcare professional promptly to mitigate the risk of complications.
Living with Claudication: Quality of Life and Support
Living with claudication can impact your daily routine and emotional well-being. It’s important to acknowledge these challenges and seek support. Minor adjustments and a strong support system can help maintain a good quality of life.
Finding ways to stay engaged with favorite activities is crucial. Creative problem-solving and exploring modifications ensure you remain active and connected to your interests. Social support from family, friends, and support groups can make a significant difference.
Consider these steps to enhance your quality of life:
- Connect with support groups for shared experiences.
- Focus on hobbies that uplift and distract you.
- Communicate openly with loved ones about your needs.
- Explore adaptive devices to aid your mobility.
- Prioritize emotional health by addressing stress and anxiety.
Seeking diverse kinds of support is central to living well with claudication.
The Psychological Impact and Seeking Support
Claudication isn’t just physical; it affects mental health, too. You might experience frustration, anxiety, or depression. Acknowledging these feelings is the first step toward managing them.
Reaching out for support is essential. Counseling or therapy can provide coping strategies. Engaging in activities that boost your mood also helps. Don’t hesitate to ask for guidance from mental health professionals. They can help create a plan to address these challenges, ensuring you don’t face them alone.
Communicating with Your Healthcare Provider
Open communication with your healthcare provider is key to managing claudication. Providing detailed information about your symptoms aids in tailoring your treatment. This partnership fosters better outcomes and adapts to your evolving needs.
Prepare for appointments by listing your questions and concerns. Discuss any lifestyle changes or medications impacting your condition. Clear communication ensures you understand treatment options and potential side effects. This ongoing dialogue promotes an active role in your healthcare and confidence in managing claudication effectively.
The Importance of Ongoing Management
Managing claudication is an ongoing process requiring commitment and regular attention. Consistent management strategies are vital in preventing further complications and ensuring an improved quality of life.
It is essential to prioritize regular follow-ups with your healthcare provider to monitor your condition. Maintaining lifestyle changes, adhering to prescribed treatments, and staying informed about advancements in care can greatly assist in managing symptoms effectively. By being proactive and adaptive, you can lead a fulfilling life despite living with claudication. Engaging with your healthcare plan facilitates better control over your health and overall well-being.
Seek Help Today!
Whether vascular or neurogenic, claudication is more than just temporary discomfort; it often indicates underlying health issues that require professional assessment and management. If you suspect you are experiencing claudication symptoms, do not ignore these warning signs. Timely medical intervention can significantly enhance your quality of life and reduce the risk of more severe complications.
We encourage you to contact Dr. Ayar at Coastal Vascular Center today. With a comprehensive approach to diagnosis and treatment, Dr. Ayar and our dedicated team can help you manage your symptoms and address the root cause of your discomfort.
Call us now at 713-999-6065 to learn more and book your appointment. Let’s walk this journey to wellness together.
Don’t let claudication hold you back. Call Coastal Vascular Center and schedule your consultation with Dr. Ayar to take your first step towards better vascular health.
Peripheral Arterial Disease Articles
Preventing Critical Limb Ischemia: Key Strategies
Critical Limb Ischemia (CLI) is a severe vascular disease that can have life-altering consequences. It's a condition marked by significant obstruction of the arteries, leading to reduced blood flow to the extremities. This can result in severe pain, non-healing...
Exploring the Link Between Rest Pain and Circulation
Rest pain is a condition that can cause significant discomfort. It's characterized by severe pain in the lower limbs, often worsening at night. This pain is not random. It's closely linked to circulation issues in the body. Peripheral arterial disease, or PAD, is a...
Understanding Causes of Leg and Ankle Swelling
Swelling in the legs and ankles is a common symptom that can be caused by a variety of conditions. It's often associated with fluid retention, a condition known as peripheral edema. Understanding the causes of this swelling is crucial for effective treatment. It...
Understanding Causes of Skin Discoloration On Legs
Skin discoloration on legs can be a puzzling and concerning symptom. It's often linked to vascular health, but what does that mean? Vascular health refers to the health of our body's circulatory system. This system made up of our heart and blood vessels, is...
Understanding Diabetes and Swollen Feet Symptoms
Understanding the link between diabetes and swollen feet can be daunting. Medical jargon can often make it challenging to grasp the specifics of this condition. This article aims to simplify the complex. It will clearly explain diabetic foot swelling, its causes,...
Understanding Atherosclerosis and Thrombosis Differences
Understanding the differences between atherosclerosis and thrombosis can be challenging. Both vascular diseases affect the blood vessels, but they have distinct characteristics. Atherosclerosis involves the buildup of plaque in the arteries. Over time, this can...